Subchondroplasty / SCP
The SCP® Procedure is a minimally-invasive surgery that targets and fills subchondral bone defects, often referred to as Bone Marrow Lesions (BML). These often-painful defects are in the spongy cancellous bone that underlies the cortical bone. The procedure is usually performed along with arthroscopy (keyhole surgery) of the nearby joint, allowing your surgeon to visualize and treat findings inside the joint.
Your surgeon will base a diagnosis of a subchondral bone defect on your clinical history, physical exam and MRI findings. A subchondral bone defect often referred to as a Bone Marrow Lesion, or BML is a term for a finding on an MRI that represents an abnormal area or defect inside the bone.
What is a Bone Marrow Lesion / BML?
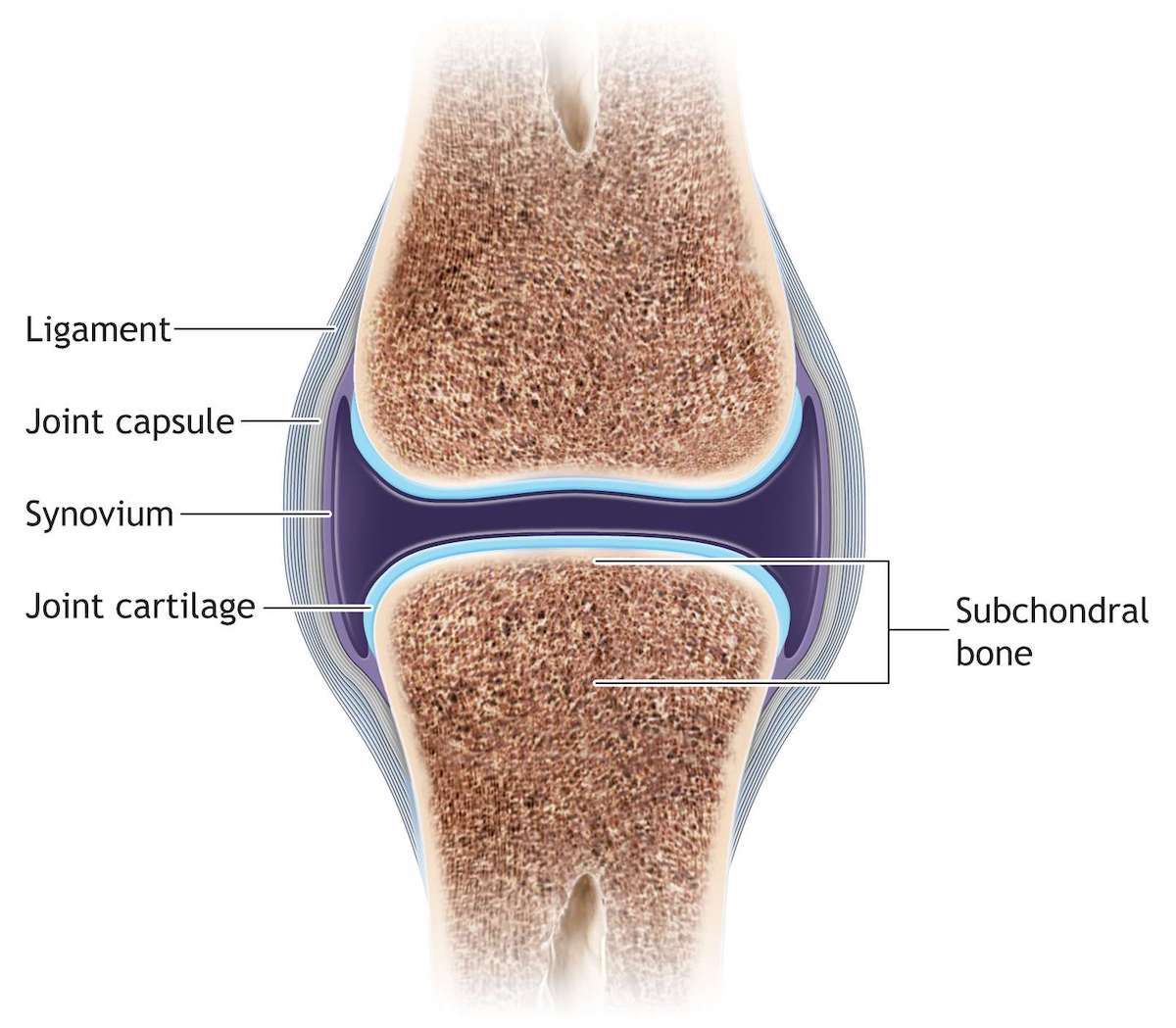
Bone marrow lesions (sometimes called Bone Marrow Edema) are small defects typically found in subchondral bone, the region below the cortical bone near a joint. They can only be seen on certain MRI sequences, appearing as a hazy white area against the background of darker bone.
Pathologists have shown that bone marrow lesions represent a healing response surrounding small defects in the subchondral bone, such as micro trabecular fractures. For that reason, the lesions can also be referred to as insufficiency fractures. This type of defect can be found throughout the extremities and pelvis. They can be found near any joint that sees weight-bearing or repetitive motion stress.

What causes a Bone Marrow Lesion/ BML?
In some cases, BML defects are a result of a bone injury that doesn’t heal properly. In other cases, BML may be a stress reaction that forms from overuse or poor joint mechanics. Other factors that correlate to chronic BML include:
Obesity and poor diet are thought to increase the likelihood of developing BML
- BML is more commonly found in middle-aged patients than in younger patients
- Patients with poor joint alignment are more likely to develop BML
- Adults who quickly increase activity may develop BML

Who is a candidate for the Subchondroplasty / SCP procedure?
You may have a defect in the bone adjacent to your joint called a chronic Bone Marrow Lesion (BML). Many surgeons believe that chronic BML will not heal without intervention. BML can only be seen on MRI. Only your doctor can tell you if you have this condition.
Discuss treatment options and potential risks with your surgeon. It is important that you fully understand all risks and benefits before making a decision to have surgery. Only your doctor can tell you if The Subchondroplasty® Procedure may be right for you. As with every surgical procedure, there are risks and potential complications. Individual results may vary. Success depends on factors such as age, weight and activity level.
How is the Subchondroplasty / SCP procedure performed?
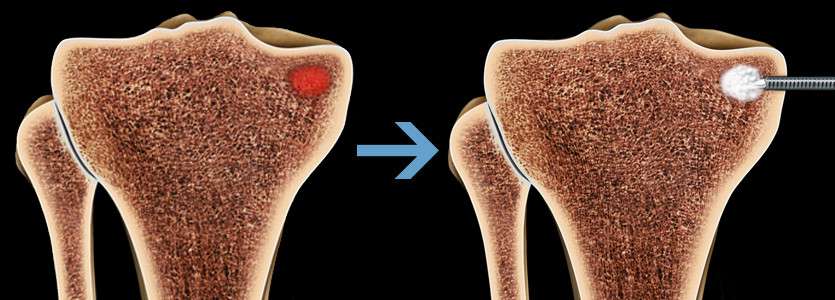
The SCP® Procedure is a minimally-invasive surgery that targets and fills chronic subchondral defects sometimes referred to as BML.
During the procedure, your surgeon will use fluoroscopy (intraoperative X-ray) to place a small, drillable cannula in the area of the bone defect. Your surgeon will then deliver AccuFill® Bone Substitute Material (BSM) into the defect, where it hardens with properties that mimic cancellous bone. During the healing process, the AccuFill® BSM is resorbed and is replaced with new bone.

What are the outcomes of the Subchondroplasty / SCP procedure?
A recent clinical study looked at 164 patients that underwent the Subchondroplasty procedure and all patients reported improved pain after the procedure, while 75% reported very little to no pain. Though results may vary, it is very promising thus far.
Bibliography
Evaluation and Management of Subchondral Calcium Phosphate Injection Technique to Treat Bone Marrow Lesion. Cartilage. 2018 Apr 1:1947603518770249. doi: 10.1177/1947603518770249. [Epub ahead of print]
Eriksen EF, Ringe JD. Bone marrow lesions: a universal bone response to injury? Rheumatol Int. 2012;32(3):575-584
Roemer FW, Neogi T, Nevitt MC, et al. Subchondral bone marrow lesions are highly associated with, and predict subchondral bone attrition longitudinally: the MOST study. Osteoarthritis Cartilage. 2010;18(1):47-53.


